Hair loss can be devastating, especially when it’s permanent. Scarring alopecia represents one of the most challenging forms of hair loss because it destroys hair follicles permanently through inflammation and fibrosis. Unlike temporary hair loss conditions, this type requires prompt diagnosis and treatment to prevent further damage. Understanding how medical professionals identify and manage scarring alopecia is essential for anyone experiencing unexplained hair loss with scalp changes.

What Primary Scarring Alopecia Means
Primary scarring alopecia, also known as cicatricial alopecia, is a group of rare disorders that destroy hair follicles and replace them with scar tissue. The term “primary” indicates that the hair follicle itself is the direct target of the destructive inflammatory process.
In primary scarring alopecia, inflammatory cells attack the upper portion of the hair follicle where the stem cells and sebaceous glands are located. This inflammation leads to permanent hair loss on scalp areas because once the follicle is destroyed and replaced with fibrous scar tissue, it cannot regenerate. The scalp may appear smooth, shiny, or slightly depressed in affected areas.
Several subtypes exist, classified according to the predominant inflammatory cell type. Lymphocytic forms include lichen planopilaris, frontal fibrosing alopecia, and discoid lupus erythematosus. Neutrophilic variants include folliculitis decalvans and dissecting cellulitis.
What Does Scarring Alopecia Look Like?
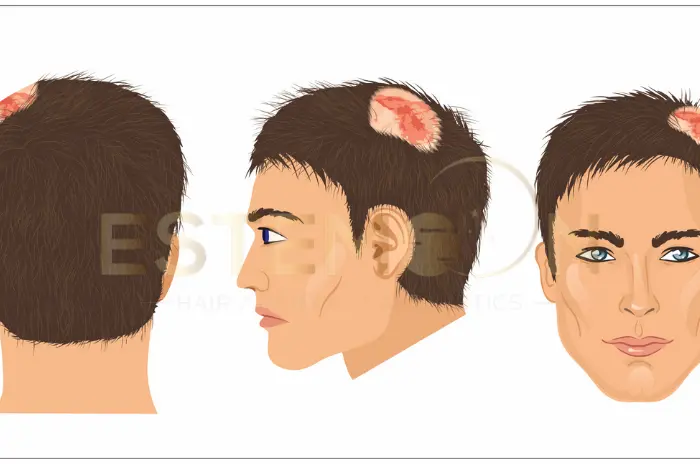
Scarring alopecia pictures reveal distinctive characteristics that help distinguish this condition from other hair loss types. The affected scalp typically appears smooth and shiny, lacking the normal follicular openings visible in healthy skin.
Patients often notice red patches on scalp hair loss during active inflammatory phases. These areas may feel tender, warm, or itchy. The scalp surface becomes permanently altered, showing a porcelain-like appearance where hair once grew.
Unlike pattern baldness, what does scarring alopecia look like varies depending on the specific type. Some forms create irregular patches of hair loss, while others follow distinctive patterns. The absence of visible hair follicle openings serves as a key diagnostic feature.
Inflammation signs include scaling, pustules, or crusting around affected areas. The scalp may show color changes, ranging from pink to dark brown, depending on skin tone and disease activity. Progressive hair loss occurs in expanding patches, often accompanied by burning scalp and hair loss sensations.
What Causes Scarring Alopecia?
Scarring alopecia causes remain partially understood, though research indicates autoimmune mechanisms play a central role. The immune system mistakenly attacks hair follicles, triggering chronic inflammation that ultimately destroys follicular structures.
Genetic predisposition contributes to disease development, with certain ethnic groups showing higher susceptibility. Environmental factors, hormonal changes, and stress may trigger or accelerate the condition in genetically susceptible individuals.
Frontal fibrosing alopecia cause specifically involves hormonal influences, particularly in postmenopausal women. Changes in estrogen levels appear to trigger this particular form of scarring alopecia. Hair care practices, including tight hairstyles and chemical treatments, may contribute to disease onset.
Infections, both bacterial and fungal, can initiate the inflammatory cascade leading to follicle destruction. Some medications and medical treatments have been associated with secondary cicatricial alopecia development.
The exact mechanisms triggering autoimmune responses against hair follicles continue to be studied. Research suggests that molecular mimicry, where immune cells mistake follicle proteins for foreign antigens, may explain the autoimmune attack.
Scarring vs Non-Scarring Alopecia Differences
Understanding the distinction between scarring and nonscarring alopecia is fundamental for proper treatment planning. These two categories differ dramatically in their mechanisms, appearance, and prognosis.
Non-scarring alopecia conditions, such as androgenetic alopecia, alopecia areata, and telogen effluvium, affect the hair shaft or temporarily disrupt the hair growth cycle without destroying the follicle itself. Hair follicles remain intact beneath the scalp surface, and follicular openings remain visible. Because the follicle structure is preserved, hair regrowth is often possible with appropriate treatment.
In contrast, scarring alopecia involves permanent hair loss through follicle destruction. The inflammatory process replaces functional follicular tissue with fibrosis hair loss scar tissue. Affected areas show decreased or absent follicular openings, and the scalp texture changes noticeably. The skin may appear smooth, shiny, or slightly atrophic.
Clinical presentation differs significantly. Non-scarring alopecias typically cause diffuse thinning or patchy hair loss without scalp surface changes. Patients rarely experience symptoms beyond cosmetic concerns.
Cicatricial alopecia symptoms often include burning, itching, pain, or tenderness in affected areas, especially during active disease phases. The scalp may show visible redness, scaling, pustules, or pigmentation changes. These symptoms reflect the ongoing inflammatory hair loss process.
Prognosis represents the most significant difference. Non-scarring alopecias offer hope for regrowth with medical treatment. Scarring alopecia treatment focuses on halting disease progression rather than reversing existing hair loss, since destroyed follicles cannot regenerate.
How Scarring Alopecia Is Diagnosed: Scalp Exam and Biopsy
Accurate alopecia diagnosis requires a systematic approach combining clinical evaluation with laboratory confirmation. The diagnostic process begins with thorough medical history and progresses to sophisticated testing methods.
Clinical Scalp Examination
The diagnostic journey starts with detailed scalp examination. Dermatologists assess hair density, distribution patterns, and scalp surface characteristics. They look for telltale signs of scarring, including loss of follicular openings, scalp texture changes, and inflammatory features like erythema or scaling.
Dermoscopy, a non-invasive technique using magnification and specialized lighting, helps visualize microscopic scalp features. In scarring alopecia, dermoscopy typically reveals decreased follicular openings, perifollicular scaling, and perifollicular erythema.
Physicians also perform a “hair pull test,” gently tugging on hair shafts to assess how easily they detach. The pattern of hair loss—whether diffuse, patchy, or in specific distributions—offers diagnostic clues about the specific type of scarring alopecia.
Scalp Biopsy Procedure
When clinical examination suggests scarring alopecia, a hair loss biopsy becomes essential for definitive diagnosis. This procedure provides tissue samples for histopathological examination, revealing microscopic changes that distinguish different types.
The standard approach involves taking two 4mm punch biopsies from active disease areas. One sample is processed for horizontal sectioning, which allows visualization of multiple follicles at various depths. The second sample undergoes vertical sectioning for traditional assessment.
The biopsy is performed under local anesthesia, takes less than 15 minutes, and leaves minimal scarring. Dermatologists select sites carefully, choosing areas showing active inflammation rather than end-stage scarring.
Histopathological examination reveals specific features that identify the scarring alopecia subtype. Pathologists assess inflammatory cell types, their location relative to follicular structures, the extent of follicle destruction, and the presence of fibrosis hair loss. These findings guide treatment selection.
Additional Diagnostic Tests
Supporting tests may include laboratory work to identify underlying systemic conditions. Blood tests can check for autoimmune markers, particularly when lupus is suspected. Direct immunofluorescence testing helps diagnose lupus-related scarring alopecia by detecting immune deposits around follicles.
Treatment Options for Scarring Alopecia: Medicines and Injections
Scarring alopecia treatment aims to halt disease progression, reduce inflammation, and preserve remaining hair follicles. While destroyed follicles cannot regenerate, aggressive treatment can prevent further permanent hair loss.
Topical Treatments
First-line therapy often includes potent topical corticosteroids applied directly to affected scalp areas. These anti-inflammatory treatment medications reduce local immune activity and inflammation. Patients typically apply these once or twice daily to active lesions.
Topical calcineurin inhibitors like tacrolimus offer alternative anti-inflammatory options with fewer long-term side effects than steroids. These medications modulate immune responses at the follicle level.
Intralesional Corticosteroid Injections
For more resistant cases, intralesional corticosteroid injections deliver medication directly into affected scalp areas. Dermatologists inject triamcinolone acetonide using fine needles at regular intervals across the involved scalp.
Injection treatments typically occur monthly or every six to eight weeks. Many patients experience significant symptom improvement and disease stabilization with this approach.
Systemic Medications
When topical and injection therapies prove insufficient, systemic medications become necessary. Oral corticosteroids can quickly control severe inflammatory hair loss but require careful management due to potential side effects.
Antimalarial drugs, particularly hydroxychloroquine, show effectiveness for lymphocytic scarring alopecias like lichen planopilaris and lupus-related hair loss. These medications modulate immune function and inflammation.
Doxycycline and other tetracycline antibiotics provide anti-inflammatory and antimicrobial benefits, particularly useful for neutrophilic forms like folliculitis decalvans.
Immunosuppressive medications such as mycophenolate mofetil, methotrexate, or cyclosporine may be prescribed for severe, refractory cases.
Emerging Therapies
JAK inhibitors represent a newer treatment class showing promise in alopecia clinical trials. These medications block specific inflammatory pathways and have demonstrated effectiveness for some types, particularly frontal fibrosing alopecia.
Biologic medications targeting specific immune molecules are being investigated. While not yet standard therapy, these treatments may offer future options for difficult cases.
Signs and Symptoms of Scarring Alopecia
Early signs of cicatricial alopecia include subtle scalp irritation, increased hair shedding, and localized tenderness. Recognizing these initial symptoms enables prompt medical evaluation and treatment initiation.
Cicatricial alopecia symptoms vary depending on disease type and activity level. Active inflammation produces burning, itching, or pain in affected areas. Patients may notice increased hair fragility and breakage before obvious hair loss becomes apparent.
Burning scalp and hair loss often occur together during inflammatory phases. The scalp may feel tight, tender, or hypersensitive to touch. Some patients describe tingling or crawling sensations in affected areas.
Visual changes include scalp redness, scaling, or pustule formation around hair follicles. The normal pattern of hair follicle openings gradually disappears as inflammation progresses. Affected areas may show color changes or textural alterations.
Progressive hair loss follows specific patterns depending on the condition type. Some forms create irregular patches, while others show characteristic distributions. The affected scalp eventually becomes smooth and shiny, lacking normal follicular structures. Advanced cases may show complete absence of hair in affected regions.
Systemic symptoms may accompany scalp changes in certain conditions. Patients with lupus-related scarring alopecia might experience joint pain, skin rashes, or fatigue. Overall health assessment helps identify underlying systemic conditions. Some patients report general malaise during active inflammatory periods.
Scarring vs non-scarring alopecia differences become apparent through careful examination. Non-scarring forms preserve follicle openings and maintain potential for regrowth, while scarring types show complete follicular destruction. This distinction proves crucial for treatment planning and prognosis determination.

When Hair Transplant May Be Considered After Disease Stability
Hair transplantation for scarring alopecia represents a complex topic requiring careful consideration. Unlike non-scarring hair loss, scarring alopecias present unique challenges.
Disease Stabilization Requirements
The fundamental prerequisite for considering hair transplant after cicatricial alopecia is complete disease quiescence. The inflammatory process must be entirely inactive for an extended period, typically at least one to two years.
Evidence of stability includes absence of symptoms, no visible scalp inflammation, stable hair loss borders without progression, and consistent negative biopsy findings. Many specialists require patients to maintain this stability while continuing maintenance medical therapy.
Suitability Assessment
Not all scarring alopecia types are equally suitable for transplantation. End-stage, completely burned-out disease with established scarring but no ongoing inflammation offers the best transplant scenario. Conditions that tend to eventually burn out, like discoid lupus erythematosus inactive for years, may be considered.
Conversely, conditions with unpredictable relapse patterns, such as lichen planopilaris or frontal fibrosing alopecia, pose higher risks. The recipient site quality matters significantly. Scarred tissue has altered blood supply and changed tissue mechanics.
Surgical Considerations
When transplantation proceeds, specialized techniques optimize success. Smaller sessions with conservative graft numbers allow assessment of tissue response. Follicular unit extraction (FUE) may be preferred to minimize surgical trauma.
Post-transplant management typically includes continuing maintenance anti-inflammatory medications indefinitely to prevent disease reactivation.
Realistic Expectations
Patients must understand that hair transplant results in scarring alopecia are generally less predictable than in non-scarring conditions. Graft survival rates may be lower, and multiple sessions might be needed. Alternative camouflage options, including scalp micropigmentation or hairpieces, may be more reliable.
Who Can Consider Hair Transplant After Scarring Alopecia Control
Determining appropriate candidates for hair restoration after scarring alopecia treatment requires comprehensive evaluation. Careful patient selection significantly impacts outcomes.
Ideal Candidate Profile
The best transplant candidates have documented disease stability for at least 18-24 months with no clinical or histological evidence of ongoing inflammation. Their scarring alopecia symptoms have completely resolved.
Ideal candidates have localized, stable scarring rather than diffuse involvement. Adequate donor hair density and quality are essential. Psychological stability and realistic expectations are crucial. Candidates must understand the limitations and risks.
Exclusionary Factors
Any evidence of active inflammation or recent disease progression disqualifies candidates. Extensive scalp scarring with poor tissue quality predicts poor graft survival. Unrealistic expectations or psychological distress focused exclusively on hair restoration may indicate poor candidacy.
Evaluation Process
Comprehensive evaluation includes detailed scalp examination by both dermatologist and hair transplant surgeon. Repeat scalp biopsy may be recommended to confirm absence of inflammation. Photographic documentation allows objective assessment of stability over time.
Discussion of alternatives ensures patients make informed decisions. Exploring non-surgical options like scalp micropigmentation or prosthetic hair systems may lead some patients to decline surgery.
Shared Decision-Making
The decision to proceed requires collaboration between patient, dermatologist, and hair restoration surgeon. All parties must agree that potential benefits outweigh risks and that the patient understands the uncertainties involved.
FAQs: Understanding Scarring Alopecia Diagnosis
How is scarring alopecia diagnosed through a biopsy?
A scalp biopsy removes small tissue samples for microscopic examination to identify inflammatory patterns and follicle destruction characteristic of scarring alopecia.
What is the key difference from nonscarring alopecia?
Scarring alopecia permanently destroys hair follicles with scar tissue replacement, while nonscarring types preserve follicles allowing potential regrowth.
Are there effective treatments for scarring alopecia?
Yes, anti-inflammatory treatments including topical steroids, injections, and systemic medications can halt disease progression and preserve remaining follicles.
Can a hair transplant work for scarring alopecia?
Hair transplant may be considered only after prolonged disease stability, though outcomes are less predictable than in non-scarring conditions.
Follow us on social media for updates, tips, and patient success stories: