Diffuse thinning is a distressing form of hair loss that affects people of all ages, creating uniform reduction in hair density across the entire scalp. Unlike other balding patterns that produce distinct patches, diffuse thinning gradually diminishes overall hair volume, making the scalp increasingly visible. This condition can significantly impact self-confidence and quality of life.
The challenge with diffuse thinning lies in its gradual progression and multiple potential triggers. From stress and hormonal imbalances to nutritional deficiencies, identifying the root cause is crucial for successful intervention. This comprehensive guide explores proven treatments and prevention methods to help you restore hair health.

What Diffuse Thinning Means for Your Hair
Diffuse thinning refers to a pattern of hair loss characterized by uniform reduction in hair density across the entire scalp rather than in localized areas. This condition differs from male pattern baldness or alopecia areata, which create distinct bald patches. With diffuse thinning, every region experiences proportional hair reduction, resulting in overall decreased volume.
In women, diffuse thinning typically presents as widening parts, reduced ponytail thickness, and increased scalp visibility while the frontal hairline remains intact. Men may experience overall volume loss either independently or combined with typical pattern baldness.
Diffuse thinning impacts the hair growth cycle at a fundamental level. Normally, 85-90% of follicles remain in active growth (anagen phase), with only 10-15% resting. Diffuse thinning disrupts this balance, pushing excessive numbers of follicles into the resting phase prematurely.
Many forms of diffuse thinning respond well to treatment, especially when addressed early. Unlike permanent scarring alopecias, diffuse thinning typically involves follicles that remain viable but function suboptimally. With proper diagnosis and targeted hair loss treatment, many people can restore significant hair density.
Main causes of diffuse thinning stress hormones nutrition
Understanding hair loss causes is essential for effective management of diffuse thinning. Multiple factors can trigger this condition, and identifying the specific cause determines the appropriate therapeutic approach.
Chronic stress ranks among the most common triggers. Prolonged psychological or physical stress elevates cortisol levels, disrupting the normal hair growth cycle. Stress-induced telogen effluvium pushes large numbers of follicles into the resting phase prematurely, resulting in noticeable hair fall 2-3 months after the stressful event.
Hormonal imbalances significantly contribute to diffuse thinning. Thyroid disorders, particularly hypothyroidism and hyperthyroidism, commonly cause widespread hair thinning. When thyroid levels become imbalanced, hair becomes dry, brittle, and prone to shedding. Women experiencing menopause, postpartum hormonal shifts, or polycystic ovary syndrome frequently develop diffuse thinning.
Androgenetic alopecia, the genetic form of hair loss, can present as diffuse thinning particularly in women with female pattern hair loss. This hereditary condition involves progressive follicle miniaturization due to genetic sensitivity to DHT. While men develop characteristic recession patterns, women often experience diffuse thinning across the crown.
Nutritional deficiencies represent a frequently overlooked but critical cause. Iron deficiency, especially low ferritin levels, is strongly associated with hair thinning particularly in women. Protein malnutrition from restrictive diets can trigger telogen effluvium. Other important factors include zinc, biotin, vitamin D, and B-vitamin deficiencies.
Medications can induce diffuse thinning as a side effect. Common culprits include beta-blockers, anticoagulants, retinoids, antidepressants, and chemotherapy agents. Anagen effluvium from chemotherapy causes rapid, severe hair loss by directly damaging actively growing follicles.
Acute illness and major physiological stressors trigger diffuse thinning through telogen effluvium. High fever, major surgery, severe weight loss, childbirth, and serious accidents all disrupt the normal hair cycle.

Early signs of diffuse thinning volume and shedding
Recognizing the early signs of diffuse thinning enables prompt intervention and better treatment outcomes. The initial symptoms are often subtle, making regular self-monitoring important.
Increased excessive hair shedding represents the most noticeable early warning sign. While normal daily hair loss ranges from 50-100 strands, people developing diffuse thinning may lose 150-300 or more strands daily. You might notice significantly more hair on your pillow, in the shower drain, on your brush, or on your clothing.
Changes in hair volume become apparent as density decreases. Your hair may feel thinner when you run your fingers through it. Ponytails and buns feel noticeably smaller in diameter. Hairstyles that previously looked full now appear flat, requiring more styling effort and products.
Increased scalp visibility emerges as hair density declines. Under bright lighting or natural sunlight, your scalp becomes progressively more visible. The part line appears wider than before. When hair is wet, the scalp shows through significantly more.
Texture changes frequently accompany diffuse thinning. Individual hair strands become finer in diameter, feeling less substantial. Hair becomes more fragile and prone to breakage. Split ends may appear more frequently despite regular trimming.
Changes in hair growth patterns provide important early clues. Hair that previously grew to a certain length now seems to stop growing shorter. The growth rate may slow noticeably.
If you observe multiple early signs persisting beyond three months, professional evaluation becomes important. A hair loss specialist can distinguish normal shedding from pathological diffuse thinning.
Diffuse thinning vs pattern baldness key differences
Understanding the distinctions between diffuse thinning and pattern baldness is crucial for accurate diagnosis and appropriate treatment selection.
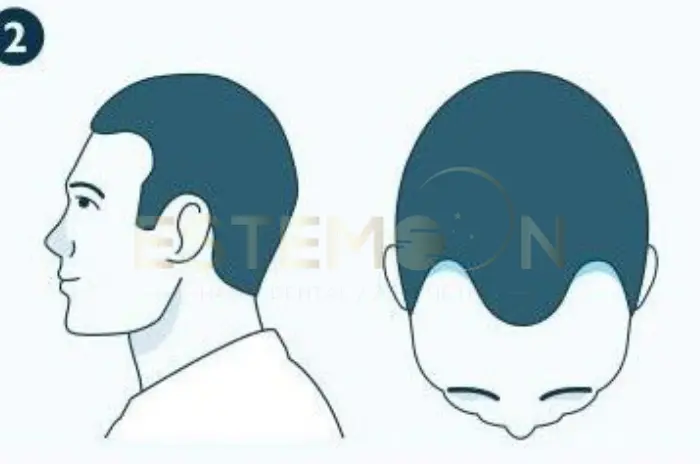
Diffuse thinning affects the entire scalp uniformly without creating distinct patterns. Hair density decreases proportionally across all regions. The hairline typically remains intact or recedes uniformly. Scalp visibility increases gradually throughout the head.
Male pattern baldness follows highly predictable patterns. Hair loss typically begins with bitemporal recession creating a characteristic M-shaped hairline, often accompanied by thinning at the vertex. These areas progressively expand and may merge, creating extensive baldness on top while leaving a horseshoe pattern.
Female pattern hair loss usually presents as diffuse thinning concentrated primarily at the crown while preserving the frontal hairline. Unlike male pattern baldness, women rarely develop complete baldness.
| Characteristic | Diffuse Thinning | Pattern Baldness |
|---|---|---|
| Distribution | Uniform entire scalp | Specific zones |
| Hairline | Maintained | M-shaped recession |
| Sides and Back | Proportionally affected | Well-preserved |
| Primary Cause | Various triggers | Genetic DHT sensitivity |
| Reversibility | Often reversible | Permanent without treatment |
The underlying causes differ substantially. Pattern baldness results primarily from genetic predisposition and DHT sensitivity. Diffuse thinning stems from numerous causes including telogen effluvium, nutritional deficiencies, hormonal imbalances, medications, and stress. Many cases are temporary and reversible.
Treatment approaches show both overlap and distinctions. Both conditions may benefit from minoxidil for hair loss. Finasteride for hair loss specifically targets DHT-mediated androgenetic alopecia. Diffuse thinning treatment emphasizes identifying and addressing the underlying trigger.
How specialists diagnose diffuse thinning exams and tests
Accurate diagnosis by a hair loss specialist is essential for effective treatment of diffuse thinning. Comprehensive evaluation involves detailed history taking, physical examination, and targeted diagnostic testing.
The consultation begins with thorough medical history focusing on the timeline of hair loss, family history, current medications, recent illnesses, dietary habits, stress levels, and menstrual history in women. This helps identify potential triggers.
Physical scalp examination provides crucial diagnostic information. The hair loss specialist assesses hair density distribution, hair shaft diameter, and scalp condition. The pull test involves grasping 50-60 hairs and pulling gently; more than 6-8 hairs coming out suggests active shedding.
Dermoscopy, a specialized magnification technique, allows detailed visualization of the scalp and hair follicles. This non-invasive examination reveals follicular patterns, hair shaft diameter variation, and signs of inflammation.
Laboratory testing identifies systemic causes. Standard blood work typically includes complete blood count, serum ferritin, thyroid function tests, vitamin D levels, and hormone panels when indicated.
Scalp biopsy provides definitive diagnosis when clinical evaluation is inconclusive. A small tissue sample is examined microscopically to assess follicle structure.
Understanding Telogen Effluvium and Hair Shedding
Telogen effluvium represents the most common cause of diffuse thinning. This condition occurs when a significant proportion of hair follicles prematurely enter the telogen (resting) phase, leading to widespread excessive hair shedding.
In normal hair cycling, approximately 85-90% of scalp follicles remain in active growth, with only 10-15% resting. Telogen effluvium disrupts this balance, pushing 30-50% or more into premature rest. Because telogen lasts 2-4 months before shedding, there’s typically a delay between the triggering event and noticeable hair fall.
Acute telogen effluvium develops suddenly following a clear triggering event. Common triggers include severe illness, major surgery, rapid weight loss, childbirth, severe stress, medication changes, and nutritional deficiencies. Shedding begins 2-3 months after the trigger and may continue for 3-6 months.
Chronic telogen effluvium involves persistent hair thinning lasting more than six months without clear triggers. This may result from ongoing nutritional deficiencies, chronic stress, or undiagnosed hormonal imbalances.
The prognosis for telogen effluvium is generally favorable. When the triggering factor is identified and eliminated, hair growth typically resumes within 6-12 months. Hair thinning treatment with minoxidil for hair loss may accelerate recovery.
Distinguishing telogen effluvium from other causes is important because it affects treatment strategy. While telogen effluvium is typically reversible, androgenetic alopecia requires ongoing treatment.
Diffuse Thinning Treatments and Prevention Tips Explained – Frequently Asked Questions
What is diffuse thinning and what does it mean?
Diffuse thinning is uniform hair density reduction across the entire scalp rather than in specific patterns, causing overall decreased volume and increased scalp visibility without distinct bald patches.
How does it differ from male pattern baldness?
Diffuse thinning affects the entire scalp uniformly including sides and back, while male pattern baldness creates specific M-shaped recession at temples and crown with preserved horseshoe pattern.
What are the main causes of diffuse thinning?
Main causes include telogen effluvium from stress or illness, hormonal imbalances including thyroid disorders, nutritional deficiencies especially iron, androgenetic alopecia, and medications.
How do specialists diagnose diffuse thinning and hair loss?
Specialists diagnose through comprehensive medical history, physical scalp examination including pull tests, dermoscopy, blood tests for nutritional and hormonal status, and sometimes scalp biopsy.
Follow us on social media for updates, tips, and patient success stories: