Hair loss can be a distressing experience, especially when it occurs suddenly or in unusual patterns. Autoimmune hair loss represents a complex category of conditions where the body’s immune system mistakenly attacks hair follicles, leading to various forms of alopecia. Understanding these conditions is crucial for proper diagnosis and treatment, as autoimmune-related hair loss often requires specialized medical approaches that differ significantly from other types of hair loss.
The relationship between autoimmune disorders and hair loss is intricate, involving multiple body systems and potentially affecting individuals of all ages. From the well-known alopecia areata to thyroid-related hair thinning, these conditions can manifest in numerous ways, each requiring specific attention and care.

Understanding Autoimmune Hair Loss and Alopecia Areata
Autoimmune hair loss occurs when the immune system incorrectly identifies hair follicles as foreign invaders and launches an attack against them. This misguided immune response disrupts the normal hair growth cycle, leading to inflammation around the follicles and subsequent hair loss. The process typically involves T-cells infiltrating the hair follicle area, creating an inflammatory environment that forces hair into the resting phase prematurely.
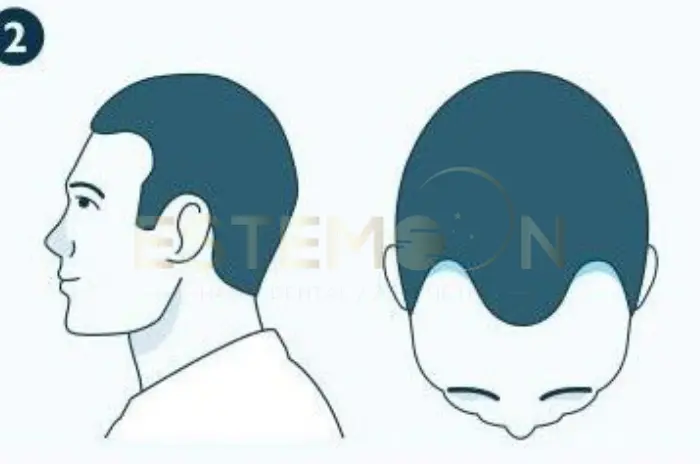
Alopecia areata stands as the most common form of autoimmune hair loss, affecting approximately 2% of the population at some point in their lives. What is alopecia areata exactly? It’s a non-scarring type of hair loss characterized by the sudden appearance of round or oval patches of complete hair loss on the scalp or other body areas. The condition can progress from small patches to more extensive hair loss, including alopecia totalis (complete scalp hair loss) or alopecia universalis (total body hair loss).
The exact triggers for alopecia areata remain unclear, but research suggests that genetic predisposition combined with environmental factors such as stress, infections, or trauma may initiate the autoimmune response. Family history plays a significant role, with about 20% of people with alopecia areata having a relative with the same condition.
Recognizing the Symptoms of Autoimmune Hair Loss
The symptoms of autoimmune hair loss vary depending on the specific condition but share certain characteristic features that distinguish them from other hair loss causes. Patchy hair loss represents the most recognizable symptom, typically appearing as smooth, round areas of complete hair loss without scaling, redness, or scarring. These patches often develop rapidly, sometimes overnight, and may be accompanied by a tingling or burning sensation.
Early warning signs include the presence of “exclamation mark” hairs around the edges of bald patches. These are short, broken hairs that are wider at the top than at the base, indicating active disease progression. Some individuals notice increased hair shedding before distinct patches appear, while others experience sudden, complete loss in specific areas without warning.
Scalp inflammation may occur in some autoimmune conditions, presenting as redness, tenderness, or scaling in affected areas. Unlike other forms of hair loss, autoimmune-related hair loss often affects areas beyond the scalp, including eyebrows, eyelashes, beard area, and body hair.

Thyroid Autoimmune Disorders and Hair Thinning
Thyroid disorders represent a significant category of autoimmune conditions that commonly cause hair loss. Both hyperthyroidism and hypothyroidism can disrupt the normal hair growth cycle, though they manifest differently. Hypothyroidism hair loss typically presents as diffuse thinning across the entire scalp, with hair becoming dry, brittle, and lacking luster. The hair loss is usually gradual and may be accompanied by thinning of the outer third of the eyebrows.
Hashimoto hair loss occurs as a result of Hashimoto’s thyroiditis, an autoimmune condition where the immune system attacks the thyroid gland, leading to hypothyroidism. This condition affects women more frequently than men and can cause significant hair thinning throughout the scalp. The hair loss associated with Hashimoto’s disease often improves with proper thyroid hormone replacement therapy, though recovery may take several months.
Hyperthyroidism hair loss and Graves disease hair loss present differently, typically causing hair to become fine, soft, and prone to breaking. The hair loss may be more noticeable during washing or brushing, and individuals may notice increased shedding throughout the day. Graves’ disease, an autoimmune condition causing hyperthyroidism, can also lead to changes in hair texture and color.
The connection between thyroid and hair loss extends beyond hormone levels. Thyroid hormones directly influence hair follicle cycling, and when levels are disrupted, the growth phase shortens while the resting phase lengthens.
Treatment Options for Autoimmune Related Hair Loss
Autoimmune hair loss treatment approaches vary significantly depending on the specific condition, severity, and individual patient factors. For alopecia areata treatment, topical corticosteroids remain the first-line therapy for limited disease, applied directly to affected areas to reduce inflammation and suppress the immune response. These treatments are most effective for small patches and early-stage disease.
Intralesional corticosteroid injections offer another effective option for localized patches, delivering medication directly to affected follicles. These injections are typically administered every 4-6 weeks and can stimulate hair regrowth in many patients. However, the treatment requires ongoing maintenance, and hair loss may recur if treatment is discontinued.
Systemic treatments become necessary for extensive hair loss or when topical treatments prove insufficient. Managing autoimmune hair loss also involves addressing underlying autoimmune conditions. For thyroid-related hair loss, proper hormone replacement therapy or antithyroid medications form the foundation of treatment.
Supportive treatments include topical minoxidil, which can enhance hair regrowth when used alongside other therapies. Light therapy, including excimer laser and narrowband UV-B, has shown promise in some studies for stimulating hair regrowth in alopecia areata patients.
Common Autoimmune Diseases That Cause Hair Loss
| Condition | Hair Loss Pattern | Associated Symptoms | Treatment Approach |
|---|---|---|---|
| Alopecia Areata | Round, smooth patches of complete hair loss | Exclamation mark hairs, possible scalp tingling | Topical/intralesional steroids, JAK inhibitors |
| Hashimoto’s Thyroiditis | Diffuse thinning throughout scalp | Fatigue, weight gain, cold intolerance, dry skin | Thyroid hormone replacement therapy |
| Graves’ Disease | Fine, brittle hair with increased shedding | Weight loss, rapid heartbeat, eye problems | Antithyroid medications, radioiodine therapy |
| Discoid Lupus | Scarring patches with permanent hair loss | Red, scaly lesions, skin discoloration | Antimalarials, topical steroids, sun protection |
| Dermatomyositis | Patchy or diffuse thinning | Muscle weakness, skin rash, joint pain | Immunosuppressive therapy, steroids |
Beyond alopecia areata and thyroid disorders, several other autoimmune conditions can lead to significant hair loss. Discoid lupus hair loss occurs in systemic lupus erythematosus, where inflammatory lesions on the scalp can cause permanent scarring and hair loss. These lesions typically appear as red, scaly patches that may leave behind areas of scarring alopecia if not treated promptly.
Dermatomyositis hair loss accompanies this rare autoimmune condition affecting muscles and skin. Hair loss in dermatomyositis may be diffuse or patchy and is often accompanied by characteristic skin changes, including the distinctive heliotrope rash around the eyes and Gottron’s papules on the knuckles.
Scleroderma hair loss results from the systemic sclerosis affecting connective tissues throughout the body. The scalp involvement can lead to scarring alopecia, particularly in areas where the skin becomes thick and tight. Early treatment is crucial to prevent permanent hair loss.
Autoimmune skin disorders and hair loss often overlap, as many conditions affecting the skin can also impact hair follicles. Lichen planopilaris, frontal fibrosing alopecia, and central centrifugal cicatricial alopecia represent examples of scarring alopecias with autoimmune components.
How Autoimmune Hair Loss is Diagnosed
Autoimmune hair loss diagnosis requires a comprehensive approach combining clinical examination, medical history, and often laboratory testing and specialized procedures. The diagnostic process begins with a thorough evaluation of the hair loss pattern, as different autoimmune conditions produce characteristic patterns that can guide initial assessment.
Hair loss diagnosis typically starts with a detailed medical history, including family history of autoimmune conditions, recent stressors, medications, and the timeline of hair loss onset. Physical examination focuses on the distribution and characteristics of hair loss, examination of remaining hairs, and assessment of the scalp condition.
Dermoscopy or trichoscopy provides detailed visualization of hair and scalp features that may not be visible to the naked eye. This non-invasive technique can identify specific patterns associated with different types of autoimmune hair loss, including the presence of exclamation mark hairs, black dots, and characteristic vascular patterns.
Laboratory testing plays a crucial role in identifying underlying autoimmune conditions. Complete blood count, thyroid function tests, antinuclear antibodies, and specific autoantibody panels help identify systemic autoimmune diseases that may be contributing to hair loss.
Key Patterns of Hair Loss in Autoimmune Conditions
Understanding the distinct patterns of hair loss in autoimmune conditions is essential for accurate diagnosis and appropriate treatment selection. Patchy hair loss characteristic of alopecia areata typically presents as well-demarcated, smooth areas of complete hair loss without inflammation or scarring. These patches may be single or multiple and can vary in size from small coin-sized areas to large confluent regions.
The progression patterns in alopecia areata can be unpredictable, with some individuals experiencing gradual expansion of existing patches while others develop new patches in different locations. The ophiasis pattern, involving hair loss along the margins of the scalp, represents a more challenging variant that often responds poorly to treatment.
Diffuse hair thinning patterns are more commonly associated with thyroid disorders and systemic autoimmune conditions. Unlike the distinct patches of alopecia areata, this pattern involves gradual thinning across the entire scalp, often with preservation of the frontal hairline.
Scarring patterns occur in more severe autoimmune conditions affecting the scalp, such as discoid lupus and lichen planopilaris. These conditions produce permanent hair loss due to destruction of hair follicles and replacement with scar tissue. Early recognition and treatment are crucial to prevent progression and preserve remaining hair follicles.
FAQs About Autoimmune Hair Loss Causes Symptoms and Treatments
How do autoimmune disorders cause hair loss?
Autoimmune disorders cause hair loss by triggering the immune system to mistakenly attack healthy hair follicles, creating inflammation that disrupts the normal hair growth cycle and forces follicles into a resting state.
What are the symptoms of autoimmune hair loss?
Symptoms include sudden appearance of round, smooth patches of complete hair loss, “exclamation mark” hairs around patch borders, possible scalp tenderness, and rapid progression of hair loss over days to weeks.
Can thyroid disease cause hair thinning?
Yes, both hyperthyroidism and hypothyroidism can cause significant hair thinning by disrupting thyroid hormone levels that are essential for normal hair follicle function and hair growth cycles.
What treatments are available for autoimmune hair loss?
Treatment options include topical and injected corticosteroids, systemic immunosuppressive medications, JAK inhibitors, topical minoxidil, light therapy, and management of underlying autoimmune conditions through specialized medical care.
Follow us on social media for updates, tips, and patient success stories: