Scarring alopecia represents one of the most challenging forms of hair loss, affecting millions worldwide. Unlike temporary hair loss conditions, this type of alopecia permanently destroys hair follicles, making early detection and treatment crucial for preventing further progression. The condition creates permanent bald patches that cannot regenerate naturally.
Understanding the complexities of cicatricial alopecia helps patients recognize warning signs and seek appropriate medical intervention. This comprehensive guide explores the various aspects of scarring alopecia, from identification to treatment approaches. Medical professionals emphasize the importance of distinguishing this condition from reversible hair loss types.
The inflammatory nature of scarring alopecia sets it apart from common baldness patterns. While male pattern baldness preserves follicle structure, scarring forms permanently eliminate regenerative capacity. This fundamental difference makes early diagnosis and intervention absolutely critical for preserving remaining hair.
What Is Scarring (Cicatricial) Alopecia?
Scarring alopecia, also known as cicatricial alopecia, is a group of hair loss disorders characterized by permanent destruction of hair follicles. The inflammatory process replaces healthy follicles with scar tissue, making hair regrowth impossible in affected areas.
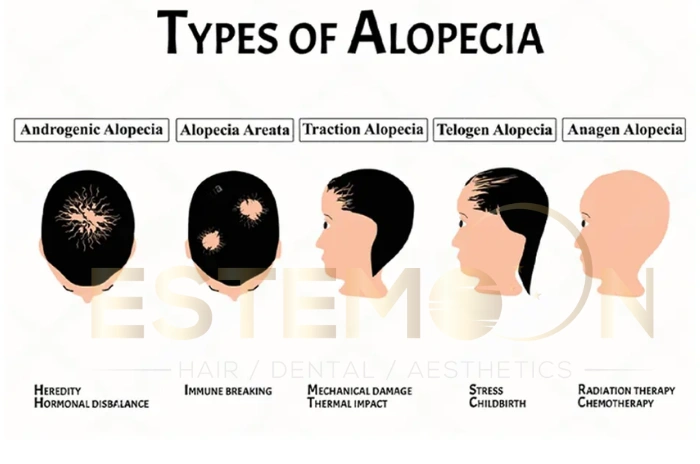
This condition differs significantly from non-scarring forms of alopecia. While conditions like androgenetic alopecia preserve follicle structure, scarring alopecia causes irreversible damage. The inflammation targets the stem cells in the hair follicle bulge region, eliminating the possibility of natural hair regeneration.
The condition affects both men and women, though certain types show gender preferences. Early intervention becomes critical because once scar tissue forms, the damage cannot be reversed. Medical professionals classify cicatricial alopecia into primary and secondary forms based on whether hair follicles are the primary target of inflammation.
Primary scarring alopecia directly attacks hair follicles, while secondary forms result from external factors like burns, infections, or trauma that secondarily damage follicles.
What Does Scarring Alopecia Look Like?
Scarring alopecia pictures reveal distinctive characteristics that help distinguish this condition from other hair loss types. The affected scalp typically appears smooth and shiny, lacking the normal follicular openings visible in healthy skin.
Patients often notice red patches on scalp hair loss during active inflammatory phases. These areas may feel tender, warm, or itchy. The scalp surface becomes permanently altered, showing a porcelain-like appearance where hair once grew.
Unlike pattern baldness, what does scarring alopecia look like varies depending on the specific type. Some forms create irregular patches of hair loss, while others follow distinctive patterns. The absence of visible hair follicle openings serves as a key diagnostic feature.
Inflammation signs include scaling, pustules, or crusting around affected areas. The scalp may show color changes, ranging from pink to dark brown, depending on skin tone and disease activity. Progressive hair loss occurs in expanding patches, often accompanied by burning scalp and hair loss sensations.
What Causes Scarring Alopecia?
Scarring alopecia causes remain partially understood, though research indicates autoimmune mechanisms play a central role. The immune system mistakenly attacks hair follicles, triggering chronic inflammation that ultimately destroys follicular structures.
Genetic predisposition contributes to disease development, with certain ethnic groups showing higher susceptibility. Environmental factors, hormonal changes, and stress may trigger or accelerate the condition in genetically susceptible individuals.
Frontal fibrosing alopecia cause specifically involves hormonal influences, particularly in postmenopausal women. Changes in estrogen levels appear to trigger this particular form of scarring alopecia. Hair care practices, including tight hairstyles and chemical treatments, may contribute to disease onset.
Infections, both bacterial and fungal, can initiate the inflammatory cascade leading to follicle destruction. Some medications and medical treatments have been associated with secondary cicatricial alopecia development.
The exact mechanisms triggering autoimmune responses against hair follicles continue to be studied. Research suggests that molecular mimicry, where immune cells mistake follicle proteins for foreign antigens, may explain the autoimmune attack.
Treatment Options for Scarring Alopecia
Scarring alopecia treatment focuses primarily on halting disease progression rather than restoring lost hair. Early intervention provides the best outcomes, as treatment cannot reverse existing scar tissue formation. The primary goal involves controlling inflammation to prevent further follicle destruction.
Anti-inflammatory medications form the cornerstone of treatment. Topical corticosteroids help reduce local inflammation and may slow hair loss progression. High-potency formulations often provide superior results compared to mild preparations. Systemic treatments including oral corticosteroids, immunosuppressants, and antimalarial drugs may be necessary for aggressive disease forms.
Intralesional steroid injections deliver medication directly to affected areas, providing targeted anti-inflammatory effects. This approach often proves more effective than topical applications for active disease. Monthly injections may be required during inflammatory phases to achieve adequate disease control.
Advanced treatments include biologics and targeted immunosuppressive therapies. These medications specifically target inflammatory pathways involved in follicle destruction. Drugs like methotrexate, cyclosporine, and mycophenolate mofetil show promise in refractory cases. Clinical trials continue investigating new therapeutic approaches including JAK inhibitors and other novel immunomodulators.
Hair regrowth after scarring alopecia remains limited once scar tissue forms. However, hair transplantation may be considered in stable disease cases. Surgical options require careful evaluation, as active inflammation can destroy transplanted follicles. Patients must demonstrate disease stability for at least two years before considering transplantation procedures.
Supportive care includes gentle scalp hygiene, sun protection, and psychological support. Alopecia support groups provide valuable emotional assistance for patients coping with permanent hair loss. Camouflage techniques, including specialized makeup and hair systems, help patients maintain confidence and quality of life.
Types of Scarring Alopecia
Types of scarring alopecia encompass several distinct conditions, each with unique characteristics and patterns. Understanding these variations helps guide appropriate treatment selection and prognosis assessment.
| Type of Scarring Alopecia | Primary Affected Areas | Demographics | Key Characteristics | Treatment Approach |
|---|---|---|---|---|
| Lichen Planopilaris | Crown and frontal scalp | Adults, both genders | Inflammatory papules, severe itching, burning sensation | Topical steroids, antimalarials |
| Frontal Fibrosing Alopecia | Frontal hairline, eyebrows | Postmenopausal women | Band-like hair loss pattern, facial hair involvement | Early intervention with anti-inflammatories |
| Central Centrifugal Cicatricial Alopecia | Crown expanding outward | Women of African descent | Hair care practice-related, genetic predisposition | Gentle hair care, topical treatments |
| Discoid Lupus Erythematosus | Variable scalp areas | Systemic lupus patients | Distinctive scaling, multi-organ involvement | Systemic lupus management |
| Folliculitis Decalvans | Vertex scalp primarily | Middle-aged adults | Pustular lesions, bacterial involvement | Antibiotics plus anti-inflammatories |
| Pseudopelade of Brocq | Irregular scalp patches | Adults, slight female preference | “Footprints in snow” appearance | Immunosuppressive therapy |
Lichen planopilaris represents the most common form, typically affecting the crown and frontal scalp areas. This condition shows characteristic inflammatory papules around hair follicles, often accompanied by severe itching and burning sensations. The inflammatory process creates a distinctive perifollicular erythema that helps distinguish it from other forms.
Frontal fibrosing alopecia primarily affects the frontal hairline and eyebrows in postmenopausal women. This condition creates a distinctive band-like pattern of hair loss along the forehead margin, often accompanied by facial hair loss. Recent research suggests hormonal changes and genetic factors contribute significantly to its development.
Central centrifugal cicatricial alopecia predominantly affects women of African descent, beginning at the crown and expanding outward. This condition often relates to hair care practices and genetic predisposition. Chemical relaxers, tight hairstyles, and excessive heat styling may trigger the inflammatory cascade in susceptible individuals.
Discoid lupus erythematosus can cause scarring alopecia as part of systemic autoimmune disease. These lesions typically show distinctive scaling and may affect other body areas beyond the scalp. Patients often require comprehensive management addressing both scalp and systemic manifestations.
Folliculitis decalvans creates pustular lesions that destroy hair follicles, often affecting the vertex scalp. This bacterial condition requires antibiotic treatment alongside anti-inflammatory therapy. The condition may show associations with Staphylococcus aureus infections requiring targeted antimicrobial approaches.
Signs and Symptoms of Scarring Alopecia
Early signs of cicatricial alopecia include subtle scalp irritation, increased hair shedding, and localized tenderness. Recognizing these initial symptoms enables prompt medical evaluation and treatment initiation.
Cicatricial alopecia symptoms vary depending on disease type and activity level. Active inflammation produces burning, itching, or pain in affected areas. Patients may notice increased hair fragility and breakage before obvious hair loss becomes apparent.
Burning scalp and hair loss often occur together during inflammatory phases. The scalp may feel tight, tender, or hypersensitive to touch. Some patients describe tingling or crawling sensations in affected areas.
Visual changes include scalp redness, scaling, or pustule formation around hair follicles. The normal pattern of hair follicle openings gradually disappears as inflammation progresses. Affected areas may show color changes or textural alterations.
Progressive hair loss follows specific patterns depending on the condition type. Some forms create irregular patches, while others show characteristic distributions. The affected scalp eventually becomes smooth and shiny, lacking normal follicular structures. Advanced cases may show complete absence of hair in affected regions.
Systemic symptoms may accompany scalp changes in certain conditions. Patients with lupus-related scarring alopecia might experience joint pain, skin rashes, or fatigue. Overall health assessment helps identify underlying systemic conditions. Some patients report general malaise during active inflammatory periods.
Scarring vs non-scarring alopecia differences become apparent through careful examination. Non-scarring forms preserve follicle openings and maintain potential for regrowth, while scarring types show complete follicular destruction. This distinction proves crucial for treatment planning and prognosis determination.
FAQs About Scarring Alopecia Symptoms, Causes and Cure Options
What is scarring alopecia and its causes?
Scarring alopecia is a permanent form of hair loss where inflammation destroys hair follicles and replaces them with scar tissue, primarily caused by autoimmune mechanisms attacking follicular structures.
Can hair regrow from scarring alopecia?
Hair cannot naturally regrow from areas affected by scarring alopecia because the follicles are permanently destroyed, though hair transplantation may be possible in stable cases.
What are the symptoms of this condition?
Scarring alopecia symptoms include permanent hair loss, scalp inflammation, burning or itching sensations, red patches, scaling, and eventual smooth, shiny skin where follicles once existed.
Can a hair transplant be a solution?
Hair transplantation may be considered for scarring alopecia patients only when the disease has been stable for at least two years and inflammation is completely controlled.




