Obesity is a global health issue affecting people of all ages and backgrounds. As traditional weight loss methods often fail to provide lasting results, bariatric surgery has become a vital option for many. This guide explores different types of bariatric procedures, offering a clear comparison to help patients make informed decisions.
Bariatric surgery has transformed the lives of millions struggling with obesity. With various procedures available, it’s essential to understand the differences, benefits, and risks before making a decision. This guide offers a detailed comparison of different types of bariatric weight loss surgery, helping patients choose the most suitable path to better health.
Gastric Bypass vs Lap Band vs Gastric Sleeve
| Procedure | Mechanism | Invasiveness | Avg. Weight Loss (1 year) |
|---|---|---|---|
| Gastric Bypass | Restriction + Malabsorption | High | 60–70% |
| Lap Band | Restriction | Low | 40–50% |
| Gastric Sleeve | Restriction | Medium | 50–60% |
- Gastric Bypass involves creating a small pouch and rerouting the intestines (restrictive and malabsorptive).
- Lap Band places an adjustable band around the upper stomach (restrictive).
- Gastric Sleeve removes part of the stomach, limiting food intake (restrictive).
How Do You Qualify for Weight Loss Surgery?
Qualifying for bariatric surgery involves a thorough medical assessment. This process ensures the patient is both physically and mentally prepared for the procedure. Criteria may vary slightly by region and healthcare provider, but the overall goal is to identify candidates who will benefit most from surgery.
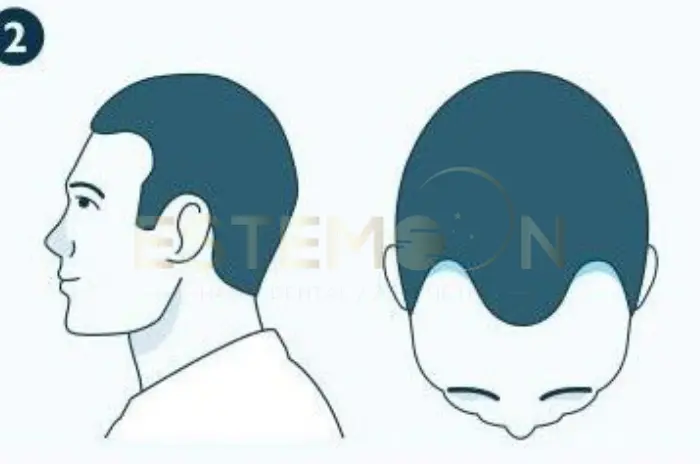
Types of Weight Loss Surgeries
Restrictive surgery
Patients undergoing restrictive procedures must adhere to a structured diet and exercise plan. The simplicity of this method makes it a common first step in surgical weight loss. However, success still heavily depends on lifestyle changes.
Malabsorptive surgery
These procedures often result in greater weight loss than restrictive methods alone. However, they also carry a higher risk of long-term nutrient deficiencies. Close monitoring by a healthcare provider is critical for patient safety.
Combination surgery
This approach offers the benefits of both mechanisms while also posing more surgical complexity. It is one of the most commonly chosen procedures worldwide. Combination surgery tends to produce faster and more sustained weight loss.

Adjustable Gastric Banding
The Procedure
During this surgery, a silicone band is placed around the upper portion of the stomach. The band creates a small pouch that limits food intake. It’s connected to a port under the skin for adjustments.
How it works
The band can be tightened or loosened by injecting saline into the port. This controls how much food passes through. The result is earlier satiety and reduced calorie intake.
Pros of gastric banding
- Minimally invasive and reversible
- Shorter recovery time
- No cutting or stapling of the stomach
Cons of gastric banding
- Slower weight loss compared to other procedures
- Frequent follow-up visits for band adjustments
- Risk of the band slipping or eroding over time
Risks of gastric banding
Possible risks include infection, nausea, vomiting, and device malfunction. Some patients may require reoperation.
Sleeve Gastrectomy
The Procedure
This surgery involves removing approximately 80% of the stomach, leaving a narrow “sleeve”-shaped pouch. It reduces the amount of food that can be eaten and lowers hunger hormone levels.
Pros of sleeve gastrectomy
- Significant weight loss within the first year
- No foreign objects or rerouting of intestines
- Shorter hospital stay compared to gastric bypass
Cons of sleeve gastrectomy
- Irreversible procedure
- Less effective for patients with severe GERD (acid reflux)
- Weight loss may be slower than with bypass
Risks of sleeve gastrectomy
Risks include bleeding, infection, leaks at the staple line, and nutrient deficiencies over time.
Gastric Bypass Surgery
The Procedure
A small pouch is created at the top of the stomach and connected directly to the small intestine, bypassing a large portion of the stomach and duodenum.
Pros of gastric bypass surgery
- Greater weight loss than with other methods
- Improvement or resolution of type 2 diabetes
- Long-term results supported by decades of data
Cons of gastric bypass surgery
- Technically complex with longer operative time
- Requires lifelong dietary changes and supplements
- Dumping syndrome may occur after sugary meals
Risks of gastric bypass surgery
Risks include infections, hernias, ulcers, and nutritional deficiencies if supplements aren’t taken consistently.

Biliopancreatic Diversion
The Procedure
This complex procedure removes a large part of the stomach and bypasses most of the small intestine. A variant called the duodenal switch retains a portion of the stomach.
Pros of biliopancreatic diversion
- Highest potential weight loss among bariatric options
- Effective for improving metabolic conditions like diabetes
Cons of biliopancreatic diversion
- High risk of nutrient malabsorption
- Requires close, lifelong medical follow-up
- Not widely available due to complexity
Risks of biliopancreatic diversion
Risks include severe vitamin and mineral deficiencies, diarrhea, and higher surgical complication rates.
Weight Loss Devices
| Device | Mechanism | Duration | Avg. Weight Loss |
| Gastric Balloon | Restricts stomach space | 6 months | 10–15% |
| Vagal Nerve Block | Inhibits hunger signals | Long-term | 5–10% |
Gastric balloon system
A temporary balloon is inserted into the stomach to take up space and promote satiety.
Pros
- Non-surgical and removable
- Short-term weight loss results
- Can serve as a bridge to surgery
Cons
- Limited duration of effectiveness (usually 6 months)
- Requires strict diet changes for success
Risks
Risks include nausea, vomiting, balloon deflation, and in rare cases, bowel obstruction.
Vagal blockade
This involves implanting a device that intermittently blocks the vagus nerve, which controls hunger signals.
Pros
- Minimally invasive
- Device can be turned off or removed
Cons
- Less weight loss compared to surgical procedures
- Requires battery-powered device maintenance
Risks
Risks include pain at the implant site, nausea, and surgical complications.

Which Weight Loss Surgery Is Best?
The best surgery varies by individual based on health status, weight loss goals, and lifestyle. A comprehensive evaluation by a bariatric team can help determine the ideal procedure. Some patients prefer less invasive methods, while others prioritize long-term results. Discuss all options with a certified specialist.
Which procedure is safer?
Generally, less invasive procedures like gastric banding or sleeve gastrectomy have lower complication rates. However, they may offer less dramatic results. Safety depends on the surgeon’s expertise and the patient’s health condition.
Which procedure has a shorter recovery time?
Lap band and gastric balloon systems offer the quickest recoveries. Sleeve gastrectomy also has a relatively short recovery period. Gastric bypass and biliopancreatic diversion require more time and lifestyle adjustments.
Which procedure is better for people with diabetes?
Gastric bypass surgery and biliopancreatic diversion show the greatest improvement or remission in type 2 diabetes. They impact gut hormones that regulate blood sugar levels. These procedures are often recommended for diabetic patients.
What are the surgical options?
Patients can choose from restrictive, malabsorptive, or combination procedures. Options include lap band, sleeve gastrectomy, gastric bypass, and biliopancreatic diversion. Non-surgical devices are also available for select cases.
What should I expect before surgery?
Pre-operative steps include nutritional counseling, psychological evaluation, lab testing, and possibly weight loss. Patients must stop smoking and adopt dietary changes to improve surgical outcomes. Insurance approval may also be required.
What should I expect after surgery?
Recovery involves diet progression from liquids to solids, vitamin supplementation, and follow-up appointments. Support groups and behavioral therapy can enhance success. Regular exercise and healthy eating habits are crucial.
How much weight can I expect to lose?
Most patients lose 50–70% of their excess weight within the first year. Results vary by procedure, adherence to post-op guidelines, and individual factors. Long-term success depends on lifestyle changes.
FAQ for Comparing The Types Of Bariatric Surgery
What are the main differences between gastric bypass, lap band, and gastric sleeve surgeries?
They differ in how they reduce stomach size and calorie absorption. Gastric bypass combines restriction and malabsorption. Lap band restricts intake with an adjustable band. Gastric sleeve reduces stomach size without intestinal changes.
How do I qualify for weight loss surgery?
You generally need a BMI of 40+, or 35+ with related health issues. Medical and psychological evaluations are required.
What are restrictive, malabsorptive, and combination weight loss surgeries?
Restrictive procedures limit food intake. Malabsorptive procedures reduce nutrient absorption. Combination procedures do both.
What are the pros and cons of adjustable gastric banding?
Pros include reversibility and shorter recovery. Cons involve slower weight loss and possible band complications.
How does sleeve gastrectomy work, and what are its risks?
It removes a portion of the stomach to limit food intake. Risks include leaks, bleeding, and vitamin deficiencies.
What are the benefits and drawbacks of gastric bypass surgery?
Lorem ipsum dolor sit amet, consectetur adipisicing elit. Optio, neque qui velit. Magni dolorum quidem ipsam eligendi, totam, facilis laudantium cum accusamus ullam voluptatibus commodi numquam, error, est. Ea, consequatur.
What is biliopancreatic diversion, and who is it suitable for?
It’s a complex procedure with high weight loss potential, suited for severely obese patients needing fast results.
What non-surgical weight loss devices are available?
Options include gastric balloons and vagal nerve blockers. They are less invasive but also less effective long-term.